Of the many different tick species found throughout the world, only a select few bite and transmit disease to humans. These maps provide general insight into the expected distribution these human-biting ticks in the contiguous United States. Populations of ticks may be found outside noted areas. Naturally occurring populations of the ticks described below do not occur in Alaska; however, the brown dog tick is endemic in Hawaii.
Note that adult ticks are the easiest to identify and male and female ticks of the same species may look different. Nymphal and larval ticks are very small and may be difficult to identify.
American dog tick (Dermacentor variabilis)
Where found: Widely distributed east of the Rocky Mountains. Also occurs in limited areas on the Pacific Coast.
Transmits: Tularemia and Rocky Mountain spotted fever.
Comments: The highest risk of being bitten occurs during spring and summer. Dog ticks are sometimes called wood ticks. Adult females are most likely to bite humans.
Blacklegged tick (Ixodes scapularis)
Where found: Widely distributed in the northeastern and upper midwestern United States.
Transmits: Lyme disease, anaplasmosis, babesiosis, and Powassan disease.
Comments: The greatest risk of being bitten exists in the spring, summer, and fall. However, adults may be out searching for a host any time winter temperatures are above freezing. Stages most likely to bite humans are nymphs and adult females.
Brown dog tick (Rhipicephalus sanguineus)
Where found: Worldwide.
Transmits: Rocky Mountain spotted fever (in the southwestern U.S. and along the U.S.-Mexico border).
Comments: Dogs are the primary host for the brown dog tick in each of its life stages, but the tick may also bite humans or other mammals.
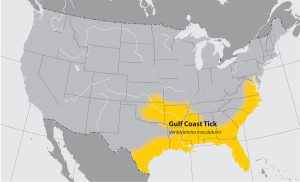
Gulf Coast tick (Amblyomma maculatum)
Where found: Coastal areas of the U.S. along the Atlantic coast and the Gulf of Mexico.
Transmits: Rickettsia parkeri rickettsiosis, a form of spotted fever.
Comments: Larvae and nymphs feed on birds and small rodents, while adult ticks feed on deer and other wildlife. Adult ticks have been associated with transmission of R. parkeri to humans.
Lone star tick (Amblyomma americanum)
Where found: Widely distributed in the southeastern and eastern United States.
Transmits: Ehrlichia chaffeensis and Ehrlichia ewingii (which cause human ehrlichiosis), tularemia, and STARI.
Comments: A very aggressive tick that bites humans. The adult female is distinguished by a white dot or “lone star” on her back. Lone star tick saliva can be irritating; redness and discomfort at a bite site does not necessarily indicate an infection. The nymph and adult females most frequently bite humans and transmit disease.
Rocky Mountain wood tick (Dermacentor andersoni)
Where found: Rocky Mountain states and southwestern Canada from elevations of 4,000 to 10,500 feet.
Transmits: Rocky Mountain spotted fever, Colorado tick fever, and tularemia.
Comments: Adult ticks feed primarily on large mammals. Larvae and nymphs feed on small rodents. Adult ticks are primarily associated with pathogen transmission to humans.
Western blacklegged tick (Ixodes pacificus)
Where found: Along the Pacific coast of the U.S., particularly northern California.
Transmits: Anaplasmosis and Lyme disease.
Comments: Nymphs often feed on lizards, as well as other small animals. As a result, rates of infection are usually low (~1%) in adults. Stages most likely to bite humans are nymphs and adult females.
While it is a good idea to take preventive measures against ticks year-round, be extra vigilant in warmer months (April-September) when ticks are most active.
Avoid Direct Contact with Ticks
- Avoid wooded and brushy areas with high grass and leaf litter.
- Walk in the center of trails.
Repel Ticks with DEET or Permethrin
- Use repellents that contain 20 to 30% DEET (N, N-diethyl-m-toluamide) on exposed skin and clothing for protection that lasts up to several hours. Always follow product instructions. Parents should apply this product to their children, avoiding hands, eyes, and mouth.
- Use products that contain permethrin on clothing. Treat clothing and gear, such as boots, pants, socks and tents with products containing 0.5% permethrin. It remains protective through several washings. Pre-treated clothing is available and may be protective longer.
Find and Remove Ticks from Your Body
- Bathe or shower as soon as possible after coming indoors (preferably within two hours) to wash off and more easily find ticks that are crawling on you.
- Conduct a full-body tick check using a hand-held or full-length mirror to view all parts of your body upon return from tick-infested areas. Parents should check their children for ticks under the arms, in and around the ears, inside the belly button, behind the knees, between the legs, around the waist, and especially in their hair.
- Examine gear and pets. Ticks can ride into the home on clothing and pets, then attach to a person later, so carefully examine pets, coats, and day packs.
- Tumble clothes in a dryer on high heat for an hour to kill remaining ticks. (Some research suggests that shorter drying times may also be effective, particularly if the clothing is not wet.)
If you find a tick attached to your skin, there’s no need to panic. There are several tick removal devices on the market, but a plain set of fine-tipped tweezers will remove a tick quite effectively.
How to remove a tick
1.Use fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
2.Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouth-parts to break off and remain in the skin. If this happens, remove the mouth-parts with tweezers. If you are unable to remove the mouth easily with clean tweezers, leave it alone and let the skin heal.
3.After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol, an iodine scrub, or soap and water.
4.Dispose of a live tick by submersing it in alcohol, placing it in a sealed bag/container, wrapping it tightly in tape, or flushing it down the toilet. Never crush a tick with your fingers.
Many tickborne diseases can have similar signs and symptoms. If you have been bitten by a tick and develop the symptoms below within a few weeks, a health care provider should evaluate the following before deciding on a course of treatment:
- Your symptoms
- The geographic region in which you were bitten
- Diagnostic tests, if indicated by the symptoms and the region where you were bitten
The most common symptoms of tick-related illnesses are:
- Fever/chills: With all tickborne diseases, patients can experience fever at varying degrees and time of onset.
- Aches and pains: Tickborne disease symptoms include headache, fatigue, and muscle aches. With Lyme disease you may also experience joint pain. The severity and time of onset of these symptoms can depend on the disease and the patient’s personal tolerance level.
- Rash: Lyme disease, southern tick-associated rash illness (STARI), Rocky Mountain spotted fever (RMSF), ehrlichiosis, and tularemia can result in distinctive rashes: ◦In Lyme disease, the rash may appear within 3-30 days, typically before the onset of fever. The Lyme disease rash is the first sign of infection and is usually a circular rash called erythema migrans or EM. This rash occurs in approximately 70-80% of infected persons and begins at the site of a tick bite. It may be warm, but is not usually painful. Some patients develop additional EM lesions in other areas of the body several days later.
◦The rash of (STARI) is nearly identical to that of Lyme disease, with a red, expanding “bulls eye” lesion that develops around the site of a lone star tick bite. Unlike Lyme disease, STARI has not been linked to any arthritic or neurologic symptoms.
◦The rash seen with Rocky Mountain spotted fever (RMSF) varies greatly from person to person in appearance, location, and time of onset. About 10% of people with RMSF never develop a rash. Most often, the rash begins 2-5 days after the onset of fever as small, flat, pink, non-itchy spots (macules) on the wrists, forearms, and ankles and spreads to the trunk. It sometimes involves the palms and soles. The red to purple, spotted (petechial) rash of RMSF is usually not seen until the sixth day or later after onset of symptoms and occurs in 35-60% of patients with the infection.
◦In the most common form of tularemia, a skin ulcer appears at the site where the organism entered the body. The ulcer is accompanied by swelling of regional lymph glands, usually in the armpit or groin.
◦In about 30% of patients (and up to 60% of children), ehrlichiosis can cause a rash. The appearance of the rash ranges from macular to maculopapular to petechial, and may appear after the onset of fever.
Tickborne diseases can result in mild symptoms treatable at home to severe infections requiring hospitalization. Although easily treated with antibiotics, these diseases can be difficult for physicians to diagnose. However, early recognition and treatment of the infection decreases the risk of serious complications. So see your doctor immediately if you have been bitten by a tick and experience any of the symptoms described here.
Material provided from the CDC http://www.cdc.gov/ticks/geographic_distribution.html















Leave a Reply